Newsroom

Announcements
Announcements
-
Events
April 15, 2024
Alzheimer’s Drug Discovery Foundation Raises $1.2 Million at Seventh Annual Memories Matter Event at American Museum of Natural History
-
Initiatives
April 1, 2024
Alzheimer’s Drug Discovery Foundation and Harrington Discovery Institute Center for Brain Health Medicines Invite Proposals for 2024 ADDF-Harrington Scholar Award
-
Events
March 18, 2024
ADDF Raises a Record-Breaking $1.5 Million at Seventh Annual Hope on the Horizon Palm Beach Dinner, Supporting Alzheimer’s Research and Drug Development
Alzheimer's Matters Blog


Developing Drugs
December 2, 2022
CTAD Showcases ADDF Leadership and Historic Progress in Alzheimer’s Research
The 2022 Clinical Trials on Alzheimer’s Disease (CTAD) conference has been a truly historic meeting, and the Alzheimer’s Drug Discovery Foundation (ADDF)’s role in bringing about a new era of research was evident throughout.

ADDF Impact
October 17, 2022
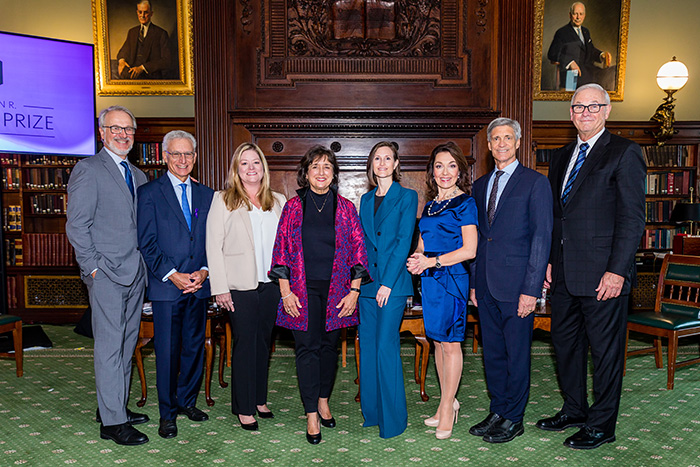
Celebrating Alzheimer’s Science and Scientists at the 2022 ADDF Goodes Prize Luncheon
Five previous winners of the prestigious Melvin R. Goodes Prize came together in New York City recently to honor this year’s winner, Miranda E. Orr, PhD, Assistant Professor of Gerontology and Geriatric Medicine at the Wake Forest University School of Medicine, and to discuss how their research is working toward the same goal – to conquer Alzheimer’s.


Protecting Brain Health
May 31, 2022
Can Lifestyle Interventions Combined with a Diabetes Drug Prevent Cognitive Decline?
Alzheimer’s Drug Discovery Foundation Funds Second Phase of Global Alzheimer’s Prevention FINGER TRIAL
Resources
Featured Video
On April 9, the ADDF celebrated its second annual Memories Matter benefit event at Chelsea Piers, which welcome nearly 600 guests and raised over $1 million for Alzheimer's research.
View more on our YouTube channel